Running’s accessibility makes it attractive to people with all types of different health and fitness goals. Both distance and speed lie solely in the eye of the beholder; however far and however fast you want to run is entirely up to you.
Despite running’s wonderful accessibility though, for some people, such as those who are experiencing pelvic organ prolapse, running isn’t as easy as lacing up a pair of trainers and getting after it.
In this post, we’ll explore how running can impact pelvic organ prolapse and share tips to prevent and manage prolapse while running.
As always, if you have specific questions about your individual circumstances, consider reaching out to a board-certified pelvic health physical therapist to improve your running experience and pelvic health.
Demystifying Prolapse: Types and Causes
Before we explore whether running can cause pelvic organ prolapse, it’s helpful to understand what, exactly, prolapse is in the first place.
Pelvic organ prolapse – or prolapse for short – is a symptom of pelvic floor dysfunction.
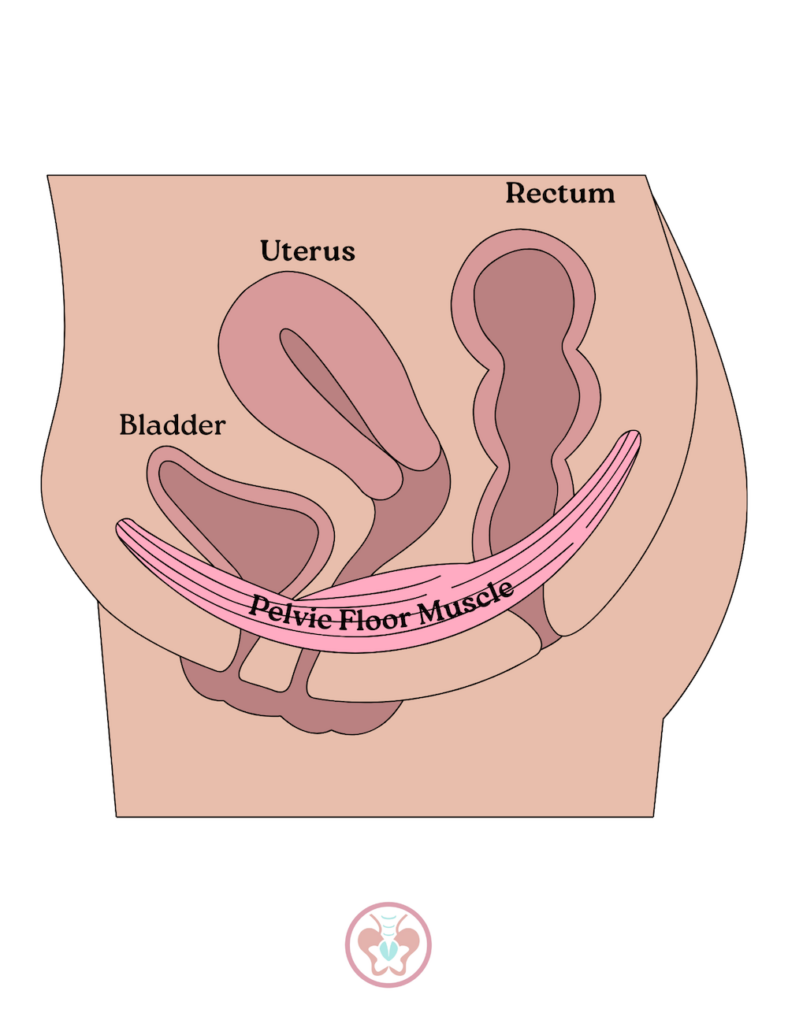
In simplest terms, pelvic floor dysfunction refers to when some aspect of the pelvic floor isn’t functioning properly.
When someone is experiencing prolapse, they may describe it as a feeling of “heaviness” or “pressure” or “fullness” in the bottom-most part of their pelvic floor or lower abdomen.
Prolapse Types: Vaginal, Bladder, and Rectal
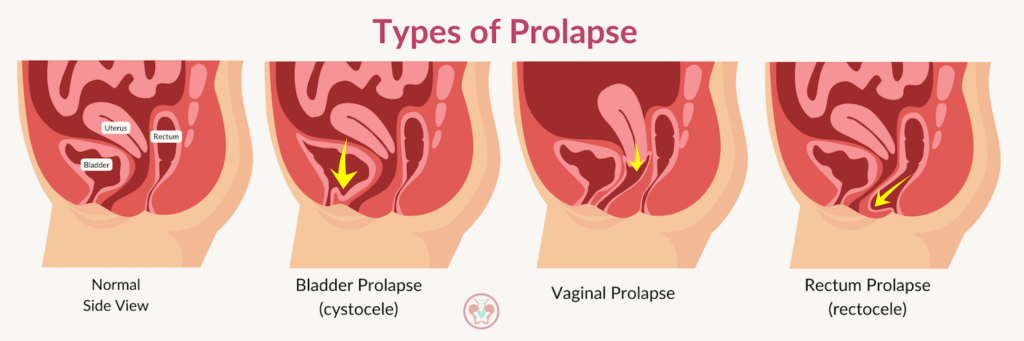
There are three different types of prolapse, demonstrated by the graphic below, and they include:
- Vaginal prolapse – when your vagina slips out of position
- Bladder prolapse (cystocele) – when your bladder sags into your vagina
- Rectal prolapse (rectocele) – when your rectum (part of your small intestine) slips down inside your anus
In jest, some people may even describe their prolapse as feeling like “everything is falling out,” which isn’t entirely untrue, actually.
As the pelvic floor musculature fails to adequately support its surrounding organs, the organs, themselves, can lose their positioning and migrate from their normal orientations to locations where they usually aren’t situated.
There are 4 stages to prolapse:
- Stage 0: no prolapse
- Stage 1: the farthest descent is less then 1 cm inside the vaginal opening
- Stage 2: the farthest descent is between 1 cm inside to 1 cm outside the vaginal opening
- Stage 3: the farthest descent is more then 1 cm outside the vaginal opening
- Stage 4: the organ wall is completely outside the vaginal opening
Prolapse Causes and Risk Factors
Prolapse is a common pelvic health malady, but of course, just because something is common does not mean that it is normal.
There are several risk factors for vaginal, bladder, and rectal prolapse that can contribute to its development.
Risk factors for bladder prolapse, vaginal prolapse, and rectum prolapse may include the following:
- Family history of prolapse
- Multiple vaginal childbirth deliveries
- Menopause
- Age
- Obesity
- Chronic constipation
- Violent/severe coughing
- Heavy lifting
- Laxative abuse
- Spinal cord problems
- Cystic fibrosis
- Dementia
- Smoking
Bladder, vaginal, and rectal prolapse share many risk factors, including age, chronic constipation, and obesity. Some are more specific to a particular type of prolapse, such as laxative abuse with rectal prolapse.
In the broadest terms possible, anytime we put exceptional amounts of pressure on our pelvic floor, we are potentially increasing our risk of developing prolapse.
Additionally, over time, as our body changes – due to pregnancy and childbirth, age, weight, or hormones, for example – our propensity to develop prolapse also changes. This is simply due to the pelvic floor musculature changing over time, which may include weakening, stretching, or tightening.
Specific to postpartum, prolapse occurs from the stretch of the pelvic floor muscles or stretch/disruption of the fascia holding the bladder.
Common Prolapse Symptoms and Signs Indicating Pelvic Floor Dysfunction
Now that we understand where pelvic floor or pelvic organ prolapse occurs and what, exactly, it entails, it’s helpful to discuss common prolapse symptoms and signs that may indicate pelvic floor dysfunction.
In the case of bladder, vaginal, or rectal prolapse, symptoms can become apparent very quickly, or they can emerge over time.
A cystocele – a symptom of a fallen bladder – occurs when someone has bladder prolapse. Over time, this may lead to urinary incontinence.
People who are experiencing bladder prolapse may actually see their bladder bulging from their vaginal opening, have difficulty fully emptying their bladder during urination, have difficulty using menstrual products, such as tampons or menstrual cups, or experience painful intercourse.
Additional symptoms of bladder prolapse can include:
- A “full” or “heavy” feeling or pain in the pelvic area that worsens while standing, lifting heavy objects, or coughing
- More frequent attempts at urination
- Difficulty fully emptying the bladder
Similarly, symptoms of vaginal prolapse vary. Some people are unaware they have vaginal prolapse until vaginal tissue from their vaginal wall actually protrudes. Some may also report pain or share that they feel like they are sitting on top of a ball. Additionally, some folks don’t know they have vaginal prolapse until it’s secondarily diagnosed in an exam by a practitioner.
More vaginal prolapse symptoms may include the following:
- A “full” or “heavy” feeling or pain in the pelvic area that worsens while standing, lifting heavy objects, or coughing
- Low back pain
- Bulging from the vagina
- Feeling like something is slipping out from the vagina
- Urinary incontinence
- Repeat bladder infections
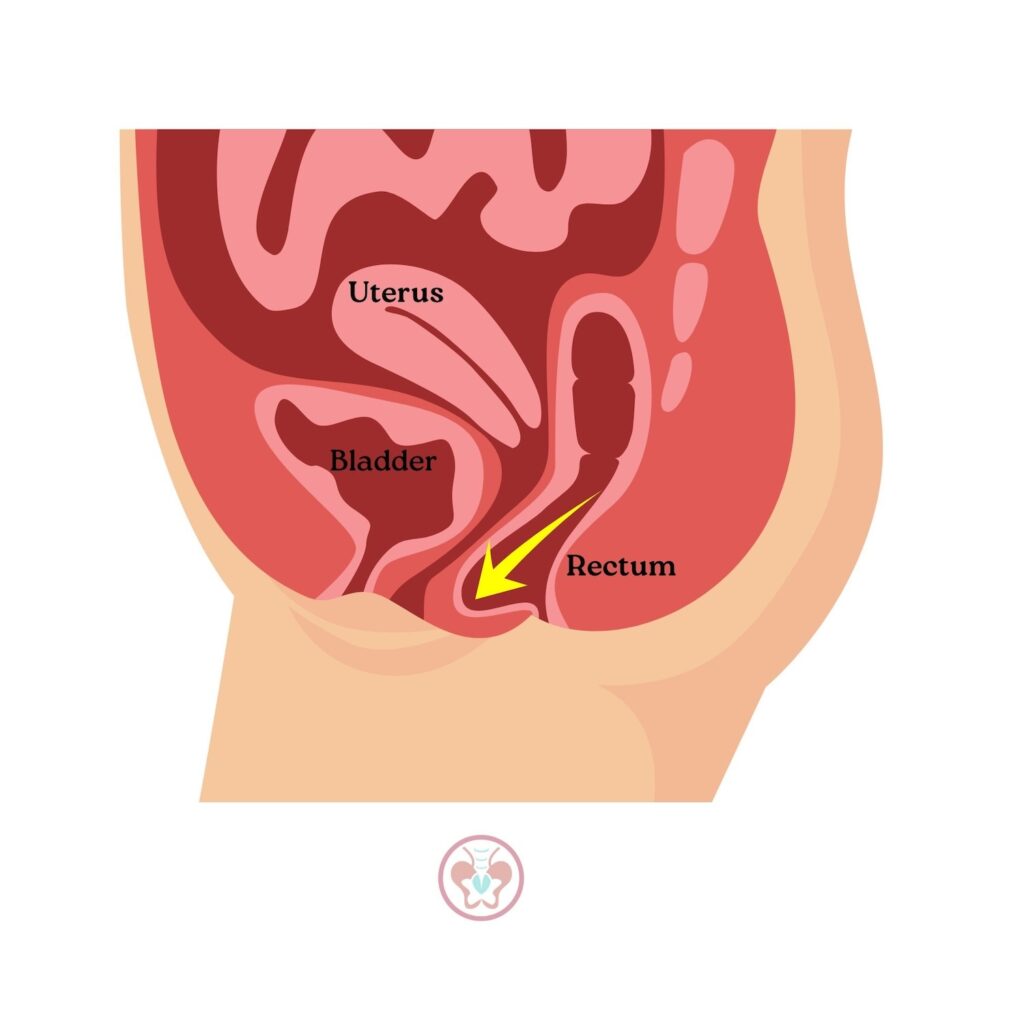
Finally, for people living with rectal prolapse, some misidentify it as looking or feeling like hemorrhoids; however, unlike hemorrhoids, rectal prolapse will not go away on its own.
Symptoms of rectal prolapse can include the following:
- Feeling pressure in the rectum
- Feeling a bulge in the anus after sneezing, heavy lifting, or coughing
- Mucus in stool
- Chronic constipation
- Chronic straining to start and/or complete a bowel movement
- Having incomplete bowel movements (sometimes due to rectocele, the weakening of the tissue wall between the rectum and vaginal wall; in severe cases, the rectum’s wall sags and bulges/protrudes into the vaginal opening)
- Abdominal discomfort or pain
- Bleeding from rectum
- Fecal incontinence
Prolapse and Running: Potential Challenges
Now that we have a more comprehensive understanding of the different types of pelvic organ prolapse and can understand the risks and symptoms associated with vaginal prolapse, bladder prolapse, and rectal prolapse, we can more fully comprehend running’s unique challenges to this pelvic floor dysfunction symptom.
Running Mechanics and Impact
We know that running, at its most basic level, is a series of one-legged hopping, over and over again. Each time our feet hit the pavement, we deliver nearly three-to-four times our body weight in force.
With this in mind, it makes sense that running can present unique challenges and risks to pelvic organ prolapse.
Our running mechanics and specifically, how we impact the ground with each footstrike, can potentially exacerbate pelvic floor issues.
Let’s break this down further.
A 150-pound runner produces nearly 600 pounds of pressure every time their feet hit the ground.
Upon impact, the pelvic floor absorbs all the stress from each footstrike.
The ground reaction force from the footstrike on the pavement transfers from the feet into the legs and quickly lands in the pelvis, our bottom-most point of the core.
When our pelvic floor is working as it should, it activates during high-impact and high-stress activities – such as running – prior to all those ground reaction forces. This is super important.
On the other hand, for folks who experience pelvic floor dysfunction like pelvic organ prolapse, running presents a unique challenge because of the repetitive groundforce battering that the pelvic floor endures with all those footstrikes. For whatever reason – and there are many! – these folks’ pelvic floors don’t activate prior to those ground reaction forces, to their detriment.
Not only is the pelvic floor taking a hit (literally, more or less) with every footstrike, it is receiving it repeatedly and at forces many times greater than the runner’s body weight.
When the pelvic floor is not sufficiently strong or adaptable to receive all these ground forces, it can result in pelvic floor dysfunction symptoms such as urinary incontinence or pelvic organ prolapse.
If the runner is already experiencing pelvic floor dysfunction, such as pelvic organ prolapse, running – in the absence of a pelvic floor physical therapy treatment and care plan – can exacerbate symptoms.
Additionally, the pelvic floor musculature is just like any other musculature elsewhere in the human body. If it is not sufficiently strong, flexible, and activated properly, its strength can become compromised over time.
In other words, running can potentially cause prolapse in runners whose pelvic floors are already compromised.
That said, the good news is two-fold:
- First, not every runner experiences pelvic organ prolapse.
- Second, there are mechanical cues that runners can heed to minimize their risk of developing pelvic organ prolapse.

Navigating Pelvic Floor Dysfunction While Running
If you’re experiencing pelvic floor dysfunction, and specifically pelvic organ prolapse, it’s critical that you think differently about how you run.
Here are some quick reminders to help mitigate your risk of developing pelvic floor dysfunction like pelvic organ prolapse from running:
- Lean forward, get your chest over your feet, and look ~30 feet in front of you on the path. In lay terms: “tits over toes”. 🙂 Looking far ahead will get your chest forward and ensure you’re not slouching. Lean from the hips, and remember that getting your chest over your toes activates your core muscles. You should feel like you’re juuuuuuuuuust on the verge of falling forward. Besides being a series of one-legged hops, running is falling forward, over and over again.
- Don’t tuck your butt, and land your feet under your body. Some runners think they need to squeeze or flex their abs when they’re running. This is completely unnecessary! Your core is engaged on its own when you run; you don’t have to do anything else. Unnecessarily flexing your abs or reaching your leg forward can contribute to urinary incontinence. Instead, your feet should land under your body. Doing so allows for better shock absorption and less pelvic stress, which, in turn, makes for a happier pelvic floor. 👍
- Mum’s the word; run quietly. When your feet strike the ground, pay particular attention to how loud it is. The louder the plod, the more likely you are creating unnecessary amounts of force. Try to instead run as quietly as possible; this audible will help remind you to only create the smallest amount of force necessary to launch you ahead in the running motion.
- Breeeeeeeeeeeeathe to support your pelvic floor. It sounds counterintuitive, but most of us probably don’t know how to breathe as well as we could… and we don’t mean taking excessively big inhales and exhales. A pelvic floor physical therapist is the best source to teach you how to breathe properly while running. This is important because proper breathing will allow you to manage intra-abdominal pressure well.
Partnering with Experts: The Role of Pelvic Floor Therapists
Reading information from experts like Dr. Janet is super helpful, yet it will only get you so far because everyone’s circumstances are different.
Truly, there is no substitute for having a real-life, in-person, board-certified pelvic floor physical therapist individually assess your specific symptoms, presentation, and lived experience to decide the best treatment plan for your pelvic organ prolapse or any other symptom of pelvic floor dysfunction.
Because prolapse can present differently depending on a person’s unique circumstances and history, it’s critical to work closely with a board-certified pelvic floor physical therapist who can best individualize treatment.
If you have pelvic organ prolapse symptoms, make an appointment to see a pelvic floor physical therapist.
Your health is absolutely worth it, and you deserve to feel the best you possibly can.
A pelvic floor physical therapist can assess your pelvic floor and symptoms and create a treatment plan to help you be the healthiest version of yourself.
We would love to help you feel better.
Please call us today so we can start your healing together.


No responses yet