We’re going to answer What is Pelvic Floor Physical Therapy.
To be fair, most people don’t know what the pelvic floor is or even if they have one in the first place … until something is wrong.
With that in mind, it’s no surprise that most people aren’t aware that pelvic floor physical therapy is “a thing” and something that can have a tremendous and profound impact on their life, especially if they are experiencing pain or discomfort or have been relegated to “just deal with it” for the rest of their lives.
Pelvic floor physical therapy is a specialized setting of physical therapy facilitated by a board certified physical therapist. At Optimize Pelvic Health, our doctors of physical therapy specialized in pelvic floor dysfunction, treat every single patient and manage their entire plan of care, from the first time they walk through the clinic door until the day they “graduate” from physical therapy.
It’s common for many physical therapy clinics to give patients about 15 minutes (out of a 60-minute appointment) with the a physical therapist, before passing them off to a physical therapist aide – usually a college student, or sometimes a high schooler – and connecting them to a therapeutic device or machine. This is the industry standard.
In contrast, at Optimize Pelvic Health, our team of physical therapists will see you for your entire appointment, each and every time. You will never be passed off to an inexperienced, under-educated aide or hooked up to a machine.
As a sub-specialty within the realm of physical therapy, pelvic floor physical therapy specifically focuses on rehabilitating muscles within the pelvic floor area, dysfunction that typically (but not always) arises due to some type of trauma or injury.
More specifically, pelvic floor physical therapy can make a dramatic difference for people who are managing their fertility, people who are pregnant, people who are postpartum, and people who are experiencing pelvic pain.
In short:
- if you are a person, and
- you have a pelvis, and
- you are experiencing some type of adversity due to pain or discomfort, or things simply feel “off,” then
- you will benefit from pelvic floor physical therapy.
At Optimize Pelvic Health, Dr. Janet and her team treat a diverse and broad spectrum of people, including but not limited to:
- patients who are trying to conceive,
- who are pregnant or postpartum, and
- patients who are experiencing any type of pain or discomfort in their pelvic floor due to injury or trauma.
What is the Pelvic Floor? Anatomy
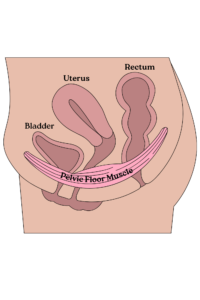
Every human on the face of this planet, regardless of gender, has a pelvic floor. It doesn’t matter if you’ve given birth; if you are a human, you have a pelvic floor.Don’t know what your pelvic floor muscles are? Most people don’t either – until or unless they experience dysfunction. The pelvic floor muscles encompass the muscles and connective tissues that support organs in your pelvis, such as your bladder, bowels (large intestine), and reproductive organs. Think of your pelvic floor like a sling; your muscles hold these organs in place while simultaneously supporting your bodily functions like peeing, pooping, and sex. If something isn’t working as it should – if it’s overly tight or weak, for example – you experience pelvic floor dysfunction. This cross-section picture below can help you visualize where, exactly, your pelvic floor is situated in your lower abdomen. If you’re like most people, until or unless you have experienced some type of problem with your pelvic floor, you have probably never thought of this incredibly important part of your body.
As is the case with the rest of our bodies, different stages of life can affect the pelvic floor differently.
For example, a pelvic floor in a person who is newly pregnant may encounter different challenges and manifest different symptoms of dysfunction than in someone who is menopausal, or a college athlete … and everyone in between.
That said, pelvic floor dysfunction can occur to anyone, regardless of gender, age, or childbearing status.
Regardless of where you are in life – pregnant, postpartum, trying to conceive, or trying to overcome some type of bodily adversity – pelvic floor physical therapy can help you become the strongest and healthiest version of yourself and help you return to the activities and hobbies you enjoy most, free from symptoms.
Pelvic Floor Dysfunction: A Primer
Because every human has a pelvic floor, everybody – regardless of gender or childbearing status — can experience pelvic floor dysfunction.
In the most general terms, pelvic floor dysfunction describes when your pelvic musculature is not working properly.
At Optimize Pelvic Health, Dr. Janet and her team see patients whose symptoms and conditions include but are not limited to the following:
- Dysuria: pain or difficulty when urinating
- constipation
- interstitial cystitis: an inflamed or irritated bladder wall whose symptoms are often mistaken for urinary tract infections
- incontinence: an inability to control the urge to urinate or defecate, resulting in urinary or fecal leakage
- unexplained lower back pain
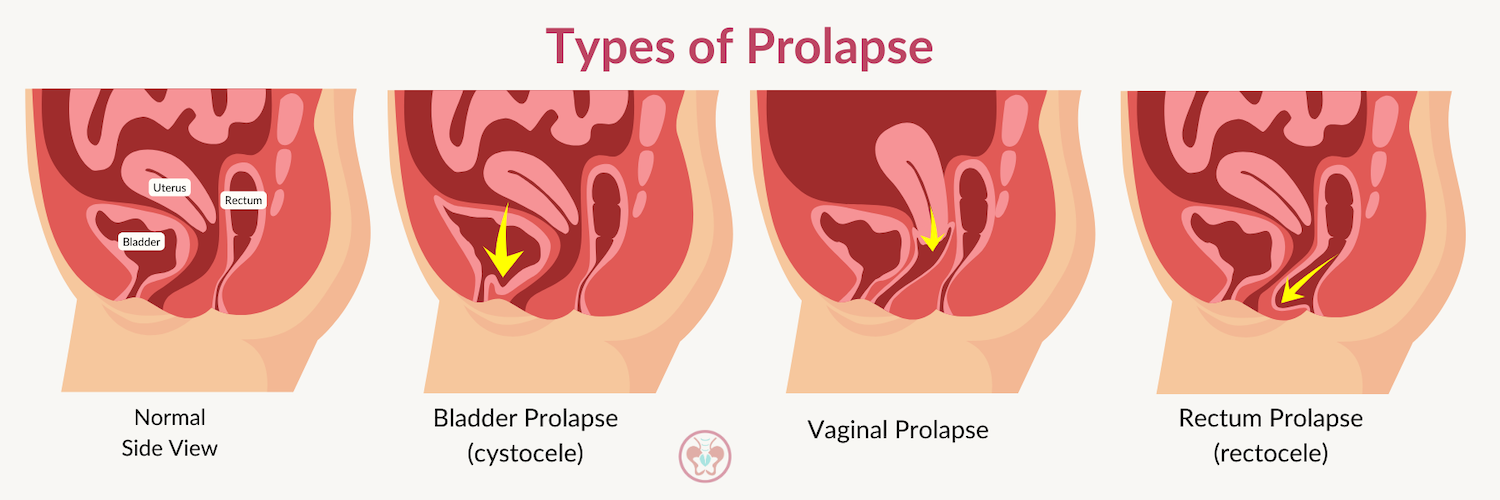
- pelvic organ prolapse: a feeling of intense pressure and heaviness because an organ housed in the pelvis (such as the bladder, uterus, or bowel) slips and bulges into the vagina
- vulvodynia: chronic pain at the vaginal opening that may result in feelings of stinging, burning, soreness, rawness, or pain during intimacy
- vaginismus: involuntary spasming or contracting of the muscles around the vagina
- dyspareunia: pain during intimacy.
How Pelvic Floor Physical Therapy Can Help
Unfortunately, for a very long time, people experiencing pelvic floor dysfunction were simply advised to Kegel their way out of their dysfunction. Precious few people knew that pelvic floor physical therapy was an option, and people lived the rest of their lives in unnecessary pain and discomfort.
Assuming that you can just Kegel your way out of any pelvic floor malady is like assuming that you can put a bandage on any “boo-boo” and that the bandage will magically fix what’s wrong.
Science and medicine don’t work that way. Despite what you may have read on the Internet otherwise, performing Kegels every day, all day, won’t absolve you of pelvic floor dysfunction. In fact, it may make matters worse.
Taking care of your pelvic health means establishing a relationship with a pelvic floor physical therapist who can diagnose your pelvic health and who can tailor your treatment plan to you.
Labor and Delivery Birth Prep
Pregnant people can benefit from pelvic floor physical therapy as they learn how to best prepare for and manage the rigorous, full-body demands of labor and delivery.
As board-certified Doctors of Physical Therapy with specializations in both pelvic health and orthopedics, Dr. Janet and her team work with their pregnant patient population to develop methods and strategies for enduring labor and delivery, including breathing techniques to lengthen the pelvic floor, pelvic floor strengthening and endurance exercises, and relaxation protocols.
Additionally, pelvic floor physical therapy can empower pregnant people in their birthing, labor, and delivery prep by teaching them how to prevent perineal tears, how to conduct perineal massages and pelvis-opening stretches, and how to breathe effectively and properly for the pushing phase.
Urinary Leakage During Pregnancy
It is the understatement of the century to say that a pregnant person’s body undergoes incredible and life-altering change during a ~40 weeks pregnancy. For many pregnant people, pregnancy-induced incontinence, or urinary leakage, becomes a part of their everyday life.
Unfortunately, many providers dismiss pregnancy-related incontinence as an irrefutable part of pregnancy, a small price pregnant people must pay as part of their growing bodily changes.
Pelvic floor physical therapy can help pregnant people who are suffering from pregnancy-related incontinence or urinary leakage.
Urinary leakage during pregnancy often results from the increasing pressure on a pregnant person’s bladder from a growing fetus. When bladders experience more pressure, they cannot hold as much urine as they used to, which often results in pregnant people needing to urinate more often than usual.
The increase in urination frequency can weaken the pelvic floor muscles, and when pelvic floor muscles are weakened, they can become more prone to leaking.
A pelvic floor physical therapist can work with a pregnant person experiencing urinary leakage to help them strengthen their pelvic floor musculature. A pelvic floor physical therapist may also work with a pregnant patient experiencing incontinence on stress management and breathing techniques, as stress can play an outsized role in the management of incontinence symptoms.
A pregnant person who is equipped with strategies and exercises from individualized pelvic floor physical therapy, such as pelvic floor strengthening exercises, stress management tools, and breathing techniques, may find that the strategies and exercises gained from pelvic floor physical therapy eliminate their urinary leakage or incontinence symptoms.
Back Pain During Pregnancy
For many people who are pregnant, previous medical providers have told them that back pain is simply part of the experience of pregnancy, much like a growing abdomen. Providers are often quick to dismiss a pregnant person’s back pain – as well as urinary leakage – as simply a universal part of the pregnancy process.
Pelvic floor physical therapists believe the opposite: pregnant people do not have to suffer unnecessarily for forty weeks (or more) with back pain.
Pregnant people who are experiencing back pain can benefit from pelvic floor physical therapy because a pelvic floor physical therapist will be able to determine if any pelvic-related symptoms or conditions are contributing to the pregnant person’s back pain.
Pain referrals from the pelvis or pelvic floor are not uncommon, and for some pregnant people, back pain can originate from excessive tension in the pelvic floor, weakness in the pelvic floor musculature, overuse injuries or muscular imbalances, or decreased pelvic floor function, among other culprits.
A board-certified pelvic floor doctor of physical therapy will be able to determine a pregnant person’s origin of back pain and can help them to manage or eradicate their symptoms completely.
Pelvic Pain During Pregnancy
Pain or discomfort in the pubic bone area for a pregnant person, also known as symphysis pubis dysfunction (SPD) or pregnancy-related pelvic girdle pain (PGP), can include a variety of uncomfortable or painful symptoms caused by pelvic joints’ stiffness or when the pelvic joints move unevenly at the front or back of the pelvis.
For many pregnant people, their symphysis pubis dysfunction results because the joint between their left and right pelvic bones (the pubic symphysis in the picture below) is allowing for more movement than is normal for them.
Ligaments loosen during pregnancy because of the hormone relaxin – which allows for pelvic bones to widen during delivery – and for some pregnant people, symphysis pubis dysfunction is a consequence of this ligament-loosening.
As is the case for urinary incontinence or urinary leakage and back pain, many pregnant people are told to simply “deal with” their symphysis pubis pain and that it’ll go away when they are no longer pregnant.
A board-certified pelvic floor doctor of physical therapy can work closely with a pregnant person to manage or eradicate their symptoms related to their symphysis pubis dysfunction or pregnancy-related pelvic girdle pain.
A pelvic floor physical therapist will work closely with the pregnant person to learn their symptoms and consider lived experiences to determine if any other bodily symptoms may be contributing to their pubis symphysis dysfunction.
In other words, a pelvic floor physical therapist will never tell a pregnant person that they must simply “deal with” their symptoms during pregnancy – be it urinary incontinence or leakage, back pain, or symphysis pubis dysfunction.
Instead, a pelvic floor physical therapist will work closely with a pregnant person to carefully consider their lived experiences and symptoms and teach them strategies, tools, and exercises to empower them to be the strongest and healthiest versions of themselves, free from symptoms, pain, and discomfort.
Postpartum Recovery
For many parents, the so-called “fourth trimester” – that early postpartum period, usually considered the first 3 or 4 or months after giving birth – can be filled with joy and wonder as they marvel at their child.
What’s talked about less often is how many parents feel burdened by anxiety, uncertainty, and even shame when it comes to talking about – and getting help for – their postpartum physical challenges.
After giving birth, patients immediately face an onslaught of information from their providers, including how to care for their baby, how to (breast)feed, how to diaper, and so much more.
It’s rare that providers walk their new parents through the most common postpartum problems, instead leaving them to figure it out on their own (3am Googling session, anyone??) and assume that their experience, while common, is “normal.”
Just 👏 because 👏 something 👏 is 👏 “common” 👏 does 👏 not 👏 mean 👏 it 👏 is 👏 “normal.” 👏
Pelvic floor physical therapy can be hugely beneficial to postpartum people who are enduring a wide variety of bodily ailments and symptoms, including but not limited to prolapse, diastasis recti (DR), urinary leakage, and pelvic pain.
Consider seeing a pelvic floor physical therapist if you’ve experienced any urinary leakage, organ prolapse, or pelvic/back/hip pain that has lasted longer than six weeks.
Pelvic floor dysfunction can feel like an “invisible” injury and oftentimes is uncomfortable and stigmatized to talk about, making it hard for patients to get the care they need.
Many postpartum-related pelvic floor dysfunctions are rectifiable by pelvic floor physical therapy; you don’t have to live in pain or discomfort unnecessarily.
Urinary Leakage Postpartum
As far as postpartum maladies go, UI is the most common. In fact, it is the most common postpartum bladder challenge Dr. Janet and her team see at Optimize Pelvic Health every single day.
At Optimize Pelvic Health, many patients – both people who have and have not been pregnant, alike – share that they leak urine when performing everyday activities like jumping, sneezing, and coughing.
Statistically speaking, at three months postpartum, 33% of patients have urinary leakage; of those, 92% will continue to have UI at one year postpartum.
Many people incorrectly believe that UI occurs when the pelvic floor muscles are weak. However, UI can occur when the pelvic floor muscles are tight.
It is important to remember that it is never too late to see a pelvic floor physical therapist if you are experiencing urinary incontinence or leakage.
Perhaps you are many months, years, or decades postpartum, or maybe you’ve never been pregnant before.
If you are experiencing urinary incontinence or leakage, you may benefit from pelvic floor physical therapy.
A board-certified pelvic floor physical therapist will work with patients to assess and diagnose their unique symptom presentations.
Additionally, pelvic floor physical therapy will help teach people who are experiencing urinary incontinence to relax their overly-tight pelvic floor musculature and may teach them other breathing techniques to eliminate abdominal pressure, diaphragmatic breathing, and retrain their “knack” reflex.
Pelvic floor physical therapists believe it is never too late to get better.
Postpartum Prolapse
A pelvic floor dysfunction that manifests postpartum for many people is a feeling of “heaviness,” which is sometimes a precursor to pelvic floor or pelvic organ prolapse.
Put simply, prolapse describes when one or more of the organs typically situated in the pelvis slips down and bulges from the vagina.
It is likely from this circumstance that many in the medical community not-so-long-ago declared outright that women were unfit for athletics because their uterus or other organs would “fall out.”
The uncomfortable feeling of migrating organs, such as the uterus, bladder, or rectum, often happens due to increasing intra-abdominal pressure.
This is especially true for running and other high-impact activities that many postpartum people are eager to return to post-pregnancy, when they are feeling undue pressure to “get their bodies back” after the birth of their child.
Sometimes though, additional non-exercise factors can increase the likelihood that athletes experience pelvic organ prolapse, such as aging, obesity, and pregnancy and vaginal delivery history.
An athlete’s pelvic floor muscles, ligaments, fascia, and connective tissues must be sufficiently strong to absorb and support rises in intra-abdominal pressure during exercise or daily activity. Otherwise, over time, they can fail, resulting in prolapse. (See also: Can Running Cause Prolapse? and How Running Form Impacts The Pelvic Floor).
When some postpartum people share their prolapse symptoms, some providers recommend that they be fitted for pessaries to “solve” their prolapse. Pessaries are nonsurgical device interventions, made of plastic or rubber, that providers or patients insert into the vagina.
Pessaries may help some patients’ prolapse in that they can help provide support to the pelvic floor and help prevent some organs from drooping and bulging into the vagina.
Nonetheless, pessaries can sometimes be an inadequate “band-aid” or “quick fix” approach to prolapse and not adequately solve the underlying issue of a weak pelvic floor.
Instead, postpartum people can get to the root of their prolapse issues and pain by seeing a board-certified pelvic floor doctor of physical therapy.
A pelvic floor physical therapist can best assess your unique symptoms and pelvic health presentation and work with you to develop a plan of care that will ultimately get you back to living and enjoying life on your own terms so you can be the healthiest version of yourself.
Postpartum Diastasis Recti (DR)
Diastasis recti (DR) refers to when the rectus abdominis muscles – often known as “the six-pack muscles” – separate during and after pregnancy.
Approximately sixty percent of pregnant and postpartum people experience diastasis recti, with nearly forty percent of postpartum people still experiencing it at six months postpartum.
A band of tissue, the linea alba, runs down the middle of the rectus abdominis musculature. During pregnancy, a pregnant person’s uterus grows to accommodate the growing fetus, which stretches the rectus abdominal muscles and thins – and sometimes pulls apart – the linea alba.
The gap between the rectus abdominis muscles can widen, sometimes resulting in a multi-finger-width gap.
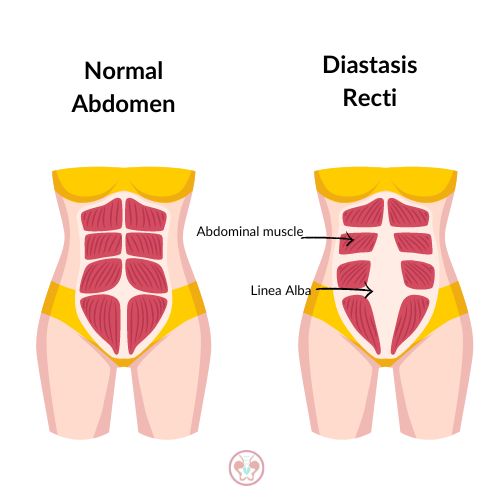
Sometimes, however, the linea alba is overstretched, loses its elasticity, and doesn’t close the gap between the right and left sides of the rectus abdominis muscles.
For some postpartum people, their bulge between their rectus abdominis muscles, usually just above or just below their navel, may make them look like they are still pregnant weeks, months, or years after giving birth.
Many people incorrectly assume that they simply need to do tons of core exercises to minimize and repair their abdominal gap. In reality, many core exercises – anything that can push a postpartum person’s abdominals outwards – are contraindicated for diastasis recti.
In other words, in an attempt to make their diastasis recti better, many postpartum people unknowingly make their diastasis recti worse by the exercises they do or attempt postpartum.
A pelvic floor physical therapist can work closely with a postpartum patient who is experiencing diastasis recti to determine if abdominal nerves are signaling the diastasis recti muscles properly.
Additionally, a pelvic floor physical therapist can help postpartum people experiencing diastasis recti (DR) by both assessing a postpartum person’s pelvic floor muscles to determine the cause of their dysfunction and teaching them which exercises they can safely perform.
Postpartum Pelvic Pain
Learning to differentiate between abdominal and pelvic pain is important for the postpartum person because the geography of the pain can help providers determine if the pain is likely a cause for serious concern.
Abdominal pain refers to pain in the middle or upper part of the abdomen, in the same area where the stomach and intestines are.
Pelvic pain, on the other hand, refers to pain in the lowest part of the abdomen, roughly situated between the hip bones (right to left) and between the navel and the pubic bone (up to down).
Perhaps unsurprisingly, two of the biggest reasons for pelvic pain postpartum is
- a ~40 week pregnancy and then
- the arduous journey of labor and delivery.
As of a result of the birthing process, a postpartum person may experience pelvic pain due to
- stretched pelvic floor muscles and nerves, from when the fetus passed through the birth canal;
- pressure on the pelvic floor due to the increasing weight of the fetus during pregnancy; and/or
- irritation to pelvic nerves during a Cesarean section.
Additionally, pregnancy-related postural changes may have occurred as the formerly-pregnant person’s baby bump grew. Once the pregnant person undergoes the birthing process, these postural changes may remain, which can contribute to a postpartum person’s pelvic pain.
Typically, pelvic pain can range from feeling “sharp and crampy,” like what many experience during their periods, that arise and abate. It may also feel like a dull, throbbing sensation..
Even if the pain is “just pain,” however, that doesn’t mean the pain is ok! If the pain persists – even in the absence of other symptoms – pelvic floor physical therapy can be helpful, particularly if the pain is limiting a postpartum person’s movement patterns or interfering with daily life activities.
Working with a board-certified doctor of physical therapy who specializes in the pelvic floor can allow a postpartum person to learn at-home remedies for comfort, such as posture cues or using supplemental aids, like a support belt.
Moreover, a pelvic floor physical therapist can provide an individualized gentle exercise treatment plan to postpartum people who are experiencing pain, in accordance with their symptoms.
Maximize the Pelvic Floor for Fertility
Infertility is a globally-felt experience, with recent studies from the World Health Organization (WHO) stating that over 17% of the adult population, one in every six adults – suffer from it.
Beyond just being a condition that describes a person’s inability to achieve a pregnancy “after 12 months or more of regular unprotected sexual intercourse” (WHO) or “after 6 months of unprotected sex” for women aged 35 years or older (CDC), infertility can adversely affect other aspects of a person’s health, too.
It’s not *just* about pregnancy.
People who suffer from infertility often experience stigma, distress, and economic hardship due to financing their fertility therapies mostly out-of-pocket, since insurance doesn’t always cover infertility treatments.
Many times, when we talk about fertility treatments, we automatically think of treatments popularized by the media, like in vitro fertilization (IVF) or intrauterine insemination (IUI).
In addition, pelvic floor physical therapy can assist and improve fertility, particularly if the infertility is caused by pelvic floor dysfunction.
Said another way: if your infertility is because something is “off” or “dysfunctional” with your pelvic floor – because something is hurting or feeling uncomfortable or tight, for example, or your pelvic floor musculature isn’t working correctly – pelvic floor physical therapy can help to remedy your dysfunction and help you improve your fertility.
Pelvic floor physical therapy includes visceral mobilization, which can be helpful in assisting with fertility. This process improves blood flow and restores organ motility (wherein every organ moves), which can help eliminate a person’s infertility.
Pelvic floor physical therapy can also address the following, which may be contributing to a person’s causes for infertility:
- Pain during sex (dyspareunia)
- Scar adhesions that limit blood flow (related to endometriosis, uterine fibroids, or post-surgical)
- Tight muscles or fascia in the pelvic floor
- Lymphatic system connections with organs not getting waste removed sufficiently
- Pelvic pain
- Nutritional deficiencies (a pelvic floor physical therapist could share evidence-based best practices for nutritional support during infertility and would refer out to a fertility-specialist dietitian for additional evidence-based guidance)
- Support for menstrual cycle tracking
Pelvic floor physical therapists are experts in the optimal functioning of all parts of the pelvic floor, so if the barrier to fertility is something “structural” in the pelvic floor, seeking out pelvic floor physical therapy can be nothing short of monumental for achieving fertility success.
Fertility and Pelvic Pain: An Understudied Connection
Pelvic floor physical therapists are clinically-trained, evidence-based medical providers who specialize in every aspect of the pelvic floor.
With the pelvic floor responsible for everything from urination, defecation, intercourse and reproduction, so it stands that pelvic floor physical therapists – who are subject matter experts in the pelvis – can be helpful partners in a person’s fertility journey.
Particularly if a person is experiencing pelvic pain, and this pain is interfering with their desires to become pregnant, pelvic floor physical therapy can hold an instrumental role in helping the person realize their fertility dream.
Moreover, pelvic floor physical therapy can play a hugely important role in helping a patient combat their infertility when it comes down to how the patient’s pelvic floor currently is (or is not) functioning.
What might this look like? Here are some examples:
- A couple has been trying to conceive for more than a year but hasn’t been successful. The patient reports that she experiences pain during sex (dyspareunia). She badly wants to have a baby, yet she utterly dreads the process because of how she feels when she and her partner have intercourse. It’s hard to look forward to “doing it” when she knows how much it’s going to hurt.
- Similarly, a couple is trying to conceive but hasn’t. The patient shares that they’ve had chronic pelvic pain ever since they experienced an accident at a young age. Their pelvic hurts all the time. The pain ranges from a dull thrum to a sharp, stabbing pain, depending on the time of the month. Intercourse worsens the pain significantly.
- A couple has been trying to conceive for a long time but has not yet succeeded. The patient shares that they have scars related to prior surgery that perhaps could be limiting blood flow, hindering their ability to conceive. They figure that they’ve had these scars for a long time, so there’s probably nothing they can do about it.
If you have been experiencing pelvic pain that may be resulting in your infertility, consider reaching out to a board-certified pelvic floor physical therapist. Because pelvic floor physical therapists are experts in the optimal functioning of all parts of the pelvic floor musculature and fascia, if there is something “structural” within the pelvic floor that may be contributing to your infertility, it can be helpful to pursue pelvic floor physical therapy.
Ready to Begin? Reach Out to Schedule an Initial Evaluation Today
If you are experiencing any type of pelvic pain or any symptoms of pelvic floor dysfunction – regardless of your childbearing status or if you’re menstruating – seeing a pelvic floor physical therapist can help to minimize or eradicate your suffering.
A pelvic floor physical therapist can assess your pelvic floor and unique symptoms and recommend a treatment plan to help you be the healthiest version of yourself.
You don’t have to live your life in pain or discomfort unnecessarily.
You don’t have to relegate yourself to “just dealing with” your symptoms for the rest of your life.
You are worth it.
Your health matters.
If you are experiencing any symptoms, please give us a call today so that we can begin your healing journey together.
